Research - Annals of Biological Research ( 2022) Volume 13, Issue 5
Received: 02-Jun-2022, Manuscript No. ABR-22-62735; Editor assigned: 06-Jun-2022, Pre QC No. ABR-22-62735(PQ); Reviewed: 16-Jun-2022, QC No. ABR-22-62735(Q); Revised: 23-Jun-2022, Manuscript No. ABR-22-62735(R); Published: 01-Jul-2022 , DOI: 10.4172/0976-1233.13.1.003
Introduction: Low Birth Weight (LBW) babies are susceptible to infections and malnutrition leading to poor physical, mental development and child morbidity. Although the health condition of Bangladesh has enriched substantially over the years, the LBW rate is still pretty high. The principal focus of this study was to examine the maternal factors (e.g. socio- demographic, and pregnancy related) affecting LBW in rural communities of Bangladeshi infants and drew a district levelprevalence map.
Methods: We used multistage sampling technique to select samples covering all the population from nine Upazilas with 233 community clinics of Rajshahi district. A total of 540 mothers and their children were enrolled into the study. Any association between LBW and maternal affecting factors were evaluated using Chi-square test with causes of LBW identified by logistic regression model.
Results: Household income-expenditure profile is statistically significant (p=0.003) with LBW where income-expenditure profile is equal. Anemia problems of the mother during pregnancy were more likely to deliver LBW babies (p=0.007). Underweight mothers had a higher probability than normal weight mothers to deliver LBW newborns (p=0.030). The mothers whose Birth interval are less than 25 months; then the risk of having LBW infants (p=0.015). Gestational age was significantly associated with LBW of babies (p=0.009). Significant relationship was found between household income - expenditure profile, maternal anemia, underweight mother, birth interval, preterm delivery with LBW.
Conclusion: This study finds various factors like, Household income-expenditure profile, Underweight mother, Birth interval, preterm delivery and anemia problems during pregnancy are momentous predictors of delivering LBW infants. Proper nourishment and monitoring on gestational length might minimize LBW.
Low birth weight, Pregnancy, Anemia, Underweight, Community clinic
An infant weighting <2500 grams (5.5 pounds) is categorized as a baby of Low Birth Weight (LBW) irrespective of of gestational age [1]. In 2019 the United Nations International Children's Emergency Fund (UNICEF) has reported that more than 20 million babies, one in seven, are born with LBW around the world [2]. In 2019 a systematic analysis depicted that more than 90% LBW were reported in low and middle-income countries [3]. Regional data demonstrate that the prevalence of LBW has the highest position in South Asia (28%), Sub-Saharan Africa (13%), Latin America (9%) and the lowest in the Pacific and Eastern Asia (6%) [4].The National LBW Survey of Bangladesh demonstrated that incidence of LBW lessened from 36% in 2004 to 22.6% in 2015 providing a sign of up gradation of the child health [5].Bangladesh Demographic and Health Survey (BDHS) in 2019 reported that the prevalence of LBW was 22.5% [6]. One of the key causes of neonatal mortality is LBW [7]. Newborns with LBW have declined cognitive, languageand motor functions [8]. Pessimistic physical consequences of LBW can scope into maturity and enhancing the risk of developing chronic diseases such as diabetes [9], post natal growth failure and respiratory diseases in their lifetime [10,11]. Additionally, infants with LBW have higher risk of stillbirth, and low Apgar score [12]. Besides, LBWbabies are at an increased risk of depression [13] and hypertension later in life [14]. LBW was related with maternaleducation and occupational status MUAC of the mother’s and maternal anemia [15- 17]. In developing countries, maternal age, antenatal care follow-up, body mass index were interpreters of LBW [18]. World Health Organization(WHO) set a goal of 30% reduction in the number of LBW by 2025 all over the world [19]. Epidemiological data onthe magnitude and allied factors had a significant contribution to plan the maternal and newborn care services [20]. Identifying risk factors for LBW has many benefits to set precautionary and treatment policy in the developmentof the health sectors of a nation. However, some studies have evaluated the risk factors with low birth weight in the context of Bangladesh based on hospital representative data or Multiple Indicator Cluster Survey (MICS) or Bangladesh Demographic Health Survey data [16, 21, 22]. This is the first time different maternal socio-demographicand reproductive, pregnancy and health service related determinants were considered to find its effect on low birth weight in the Northern region of Bangladesh. Therefore the aim of this study is to investigate the incidence of LBW and accentuated explanatory factors (e.g. maternal socio-demographic, reproductive, pregnancy and health service connected) affecting LBW in the population of Bangladesh based on the representative data collected from the Rajshahi District. Hopefully this study would evaluate the nation’s improvement towards SDG-3, and contribute in public health policy, and mediation, and which in turn would help in reducing the prevalence of LBW in Bangladesh.
The required data for this cross-sectional study was collected directly from the field survey conducted in October- December 2016 at the community clinics in Rajshahi district. Rajshahi district is in the north-western part of Bangladesh. The total area of the district is 2425.37 square km and the population is 2.7 million (BSS, 2011, adjusted on 16 March 2012) including the 17.33% urban and 82.67% rural population.
Inclusion criteria
The respondents of this study were the mothers who were living at the catchment area of a community clinic in the district. All selected respondents were interviewed by an expert community health worker.
Sample size determination
Multistage sampling technique was utilized to select the samples and the following formula has been used for collecting the samples:
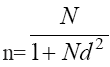
where, n=sample size, N=household size (in here 2,71,302) and d=marginal error (we considered, d=0.05). 95% confidence level has been considered in this study. This formula provided that 399 samples were required for this study. However, 540 samples were considered in this study and their information was collected to fulfill the research objective.
Sample selection procedure
A total of 233 community clinics are providing their services in nine Upazilas of the Rajshahi district (BBS, District Statistics, 2011). Multistage sampling technique was used to collect the samples covering all the population from these Upazilas. In the first stage of sampling, 2 community clinics were selected from each Upazila taking into account all the community clinics by simple random sampling. In the second stage, 2 villages were selected from the catchment areas (one is nearest and another is a far distance village) of the community clinic. Thirdly, all the households of the selected villages that have under-5 children were identified by their identification number (holding number or listing) and then 15 households were selected from each village by simple random sampling, constituting a total of 540 households. From each household, the mother of the household had interviewed as a respondent.
Outcome variable
Child birth weight was the outcome variable of this study which was divided into two categories (i) low birth weight (LBW), indicated a birth weight less than 2500 gm, defined as very small or smaller than average size (coded, 1); (ii) normal birth weight (NBW), indicated a birth weight 2500 gm or (2500-4200) gm, defined as average or above (coded, 0) (WHO, 2016) [1].
Exposure variables
The explanatory variables are scheduled under with their classification within parenthesis.
Maternal socio-demographic variables
Household marginalized group (No,Yes); Household vegetable garden (No, Yes); Household income-expenditure profile (Surplus, Equal, Sometimes deficit, Always deficit); Sleep under treated mosquito net (No, Yes); Household drinking water facility (Improved, Unimproved); Mother age group (Adolescent, Non-adolescent); Mother BMI (Underweight, Normal weight); Education level of the mothers (Below high school, Plus high school); Occupation of the mothers (Housewife, Others).
Maternal reproductive and pregnancy variables
Birth interval (in months) (Less than 25, Greater than or equal 25); High fever problems (No, Yes); Anemic mother (No, Yes); Vaginal bleeding problems (No, Yes); Taking Iron folic supplementary (No, Yes).
Maternal health service variables
Number of ANC visits (<4 times, ≥ 4 times); Delivery place (Home, Govt. hospital/Private clinic); Gestational age at delivery (Full term delivery, Preterm delivery); Child Sex (Boy, Girl). Most of the exposure variables had been identified as the source of prior studies [15-18].
Anthropometric measurement
A portable stadiometer and digital scales were used to measure the women’s weight and height, respectively. Using the techniques of Martin and Saller [23], an individual’s height was measured by standing on the machine without shoes, looking straight ahead and keeping shoulders level and weight measured wearing thin clothes. Weight and height were measured in the unit of Kilogram (kg) and meter (m), respectively. Body mass index was determined using the formula according to WHO (2004) formula, which is:
BMI=weight (kg)/height (m2)
According to, the gestational age at delivery is categorized as preterm delivery (<37 weeks) and full term delivery (≥ 37 weeks).
Statistical analysis: Descriptive measurements were used to enunciate the overall situations of the study variables in this study. To find out the association between low birth weight among mothers and their socio-demographic, reproductive, pregnancy and health service related factors were analyzed by χ2-distribution. Binary logistic regression was used in the present study to find the overall effects of the maternal socio-demographic, reproductive, pregnancy and health services related factors on LBW among mothers. Standard Error (SE) was used to detect the multicollinearity problem among exposure factors for multiple logistic regression models [24]. Statistical significance was accepted at p<0.05. The whole analysis of this study is completed with the statistical software named Statistical Package for Social Sciences (SPSS), version IBM 20, to reach our objectives.
The percentage of Low Birth Weight (LBW) was 10% in Rajshahi district during the survey period Figure 1.The univariate and bivariate distributions of LBW according to the maternal socio-demographic, reproductive, pregnancy and health service related factors were given in Table 1. It is observed from the chi-square distribution Table 1 that the LBW in Rajshahi district, Bangladesh is significantly (p=0.030) associated with the Household income-expenditure profile where 14.9% chance of having a LBW child for the mothers whose Household income-expenditure profile is equal. Furthermore, Household drinking water facility statistically significant (p=0.030) with LBW. There was an 11.0% chance of having a LBW child for the mothers who were drinking unimproved water. BMI of the mothers is also a significant (p=0.043) predictor of the LBW in the study area. There was a 15.6% chance of having a LBW child for the mothers who were in underweight status according to their BMI. LBW is significantly (p=0.011) related to the birth interval with a 19.0% chance of having a LBW child for the mothers who take less than 25 months birth interval. It is observed that if the mothers’ have anemia problems during their pregnancy period (36.4%), then they have a significant (p=0.003) chance of having a LBW child. It is also noticed that the percentage of LBW is significantly low (p=0.049) if the place of delivery is the Govt. Hospital/Private clinic (11.9%). On the other hand the gestational age at delivery is one of the most significant (p=0.001) factors of the LBW in Rajshahi district, Bangladesh. There was a 20.3% chance of having a LBW child if the gestational age at delivery was less than 37 weeks (preterm delivery). From Table 2 it is shown that the probability of LBW of the neonates among the mothers who have anemia problems during the pregnancy period had 6.50 times higher than the neonates whose mothers have not anemia problems during the pregnancy period (AOR=6.50, 95% CI=1.65-25.50, p=0.007). The gestational age at delivery is less than 37 weeks (preterm delivery) then there are 2.50 times higher probability of having the low birth weight neonates among the mothers (AOR=2.50, 95% CI=1.26-4.96, p=0.009). The mothers whose Birth interval is less than 25 months had 2.63 times higher chance of having the low birth weight neonates than the mothers whose Birth interval is greater than or equal 25 months (AOR=2.63, 95% CI=1.21-5.70, p=0.015). Again the mothers whose BMI status is underweight had 2.14 times higher probability of having the low birth weight neonates than the mothers whose BMI status is normal weight (AOR=2.14, 95% CI=1.07-4.25, p=0.030). On the other hand if the household income-expenditure profile is equal then there are 3.98 times higher underwent low birth weight infants among the mothers (AOR=3.98, 95% CI=1.59-9.94, p=0.003).
| Study variable | Total, N | Child birth weight | χ2-value | p-value | |
|---|---|---|---|---|---|
| Normal birth weight(≥2500gm), N (%) | Low birth weight (<2500gm), N (%) | ||||
| Socio-demographic factors of the Mothers | |||||
| Household marginalized group | 3.141 | 0.076 | |||
| No | 468 | 417 (89.1) | 51 (10.9) | ||
| Yes | 72 | 69 (95.8) | 3 (4.2) | ||
| Household vegetable garden | 2.751 | 0.097 | |||
| No | 388 | 344 (88.7) | 44 (11.3) | ||
| Yes | 152 | 142 (93.4) | 10 (6.6) | ||
| Household income-expenditure profile | 8.942 | 0.030 | |||
| Surplus | 139 | 132 (95.0) | 7 (5.0) | ||
| Equal | 181 | 154 (85.1) | 27 (14.9) | ||
| Sometimes deficit | 181 | 165 (91.2) | 16 (8.8) | ||
| Always deficit | 39 | 35 (89.7) | 4 (10.3) | ||
| Sleep under treated mosquito net | 3.409 | 0.065 | |||
| No | 100 | 95 (95.0) | 5 (5.0) | ||
| Yes | 440 | 391 (88.9) | 49 (11.1) | ||
| Household drinking water facility | 4.684 | 0.030 | |||
| Improved | 56 | 55 (98.2) | 1 (1.8) | ||
| Unimproved | 484 | 431 (89.0) | 53 (11.0) | ||
| Mother age group | 0.003 | 0.957 | |||
| Adolescent | 41 | 37 (90.2) | 4 (9.8) | ||
| Non-adolescent | 499 | 449 (90.0) | 50 (10.0) | ||
| Mother BMI | 4.105 | 0.043 | |||
| Underweight | 96 | 81 (84.4) | 15 (15.6) | ||
| Normal weight | 444 | 405 (91.2) | 39 (8.8) | ||
| Education level of the mothers | 0.257 | 0.612 | |||
| Below High School | 197 | 179 (90.9) | 18 (9.1) | ||
| Plus High School | 343 | 307 (89.5) | 36 (10.5) | ||
| Occupation of the mothers | 2.308 | 0.129 | |||
| Housewife | 520 | 466 (89.6) | 54 (10.4) | ||
| Others | 20 | 20 (100.0) | 0 (0.0) | ||
| Reproductive and pregnancy related factors of the Mothers | |||||
| Birth interval (in months) | 6.487 | 0.011 | |||
| Less than 25 | 63 | 51 (81.0) | 12 (19.0) | ||
| >= 25 | 477 | 435 (91.2) | 42 (8.8) | ||
| High fever problems | 0.387 | 0.534 | |||
| No | 465 | 420 (90.3) | 45 (9.7) | ||
| Yes | 75 | 66 (88.0) | 9 (12.0) | ||
| Anemic mother | 8.672 | 0.003 | |||
| No | 529 | 479 (90.5) | 50 (9.5) | ||
| Yes | 11 | 7 (63.6) | 4 (36.4) | ||
| Vaginal bleeding problems | 1.403 | 0.236 | |||
| No | 524 | 473 (90.3) | 51 (9.7) | ||
| Yes | 16 | 13 (81.2) | 3 (18.8) | ||
| Taking Iron folic supplementary | 2.023 | 0.155 | |||
| No | 51 | 43 (84.3) | 8 (15.7) | ||
| Yes | 489 | 443 (90.6) | 46 (9.4) | ||
| Health service related factors of the Mothers | |||||
| Number of ANC visit | 0.545 | 0.460 | |||
| < 4 times | 440 | 394 (89.5) | 46 (10.5) | ||
| >= 4 times | 100 | 92 (92.0) | 8 (8.0) | ||
| Place of delivery | 3.876 | 0.049 | |||
| Home | 196 | 183 (93.4) | 13 (6.6) | ||
| Govt. hospital/ Private clinic | 344 | 303 (88.1) | 41 (11.9) | ||
| Gestational age at delivery | 10.809 | 0.001 | |||
| Full term delivery(≥37 weeks) | 461 | 423 (91.8) | 38 (8.2) | ||
| Preterm delivery(<37 weeks) | 79 | 63 (79.7) | 16 (20.3) | ||
| Child Sex | 0.896 | 0.344 | |||
| Boy | 273 | 249 (91.2) | 24 (8.8) | ||
| Girl | 267 | 237 (88.8) | 30 (11.2) | ||
Notes: CM: Centimeter; ‘BMI: Body Mass Index; ANC: Anti Natal Care; gm: Gram
Table 1. Univariate and bivariate distributions of low birth weight of neonates in Rajshahi district according to the maternal socio-demographic, reproductive, pregnancy and health service related factors
| Characteristic | Low birth weight | |||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | |||||
| OR | (95 % CI) | p-value | AOR | (95 % CI) | p-value | |
| Household income-expenditure profile | ||||||
| Surplus® | 1.00 | 1.00 | ||||
| Equal | 3.31 | 1.39-7.84 | 0.007 | 3.98 | 1.59-9.94 | 0.003 |
| Sometimes deficit | 1.83 | 0.73-4.58 | 0.197 | 2.10 | 0.80-5.50 | 0.129 |
| Always deficit | 2.15 | 0.59-7.78 | 0.241 | 2.72 | 0.70-10.58 | 0.148 |
| Household drinking water facility | ||||||
| Improved | 0.15 | 0.02-1.09 | 0.061 | 0.18 | 0.02-1.36 | 0.096 |
| Unimproved® | 1.00 | 1.00 | ||||
| Mother BMI | ||||||
| Underweight (< 18.5 kg/m2) | 1.92 | 1.01-3.65 | 0.046 | 2.14 | 1.07-4.25 | 0.030 |
| Normal weight ® (18.5-24.99 kg/m2) | 1.00 | 1.00 | ||||
| Birth interval (in month) | ||||||
| Less than 25® | 1.00 | 1.00 | ||||
| >= 25 | 2.44 | 1.20-4.93 | 0.013 | 2.63 | 1.21-5.70 | 0.015 |
| Anemic mother | ||||||
| No® | 1.00 | 1.00 | ||||
| Yes | 5.47 | 1.55-19.35 | 0.008 | 6.50 | 1.65-25.50 | 0.007 |
| Birth place | ||||||
| Govt. hospital/ Private clinic | 0.53 | 0.27-1.06 | 0.052 | 0.52 | 0.26-1.05 | 0.068 |
| Home® | 1.00 | 1.00 | ||||
| Gestational age at delivery | ||||||
| Full term delivery (≥37 weeks)® | 1.00 | 1.00 | ||||
| Preterm delivery (< 37 weeks) | 2.83 | 1.48-5.37 | 0.001 | 2.50 | 1.26-4.96 | 0.009 |
Notes: cm: Centimeter; BMI: Body Mass Index; ®: Reference Category; AOR: Adjusted Odds Ratio; CI: Confidence Interval
Globally, Low Birth Weight (LBW) is one of the significant public health burdens in the 21st century. LBW is a crucial determinant of morbidity and mortality among newborn babies in Bangladesh [25]. The study depicts the incidence and maternal demographic, pregnancy and health service risk factor of LBW in Rajshahi district, Bangladesh. Our f indings explored that almost one out of every ten infants born is a baby with LBW. In 2018 this rate was 11% in that district [26]. Hence the results of this study imply that Bangladesh’s LBW rate is in line with developed countries, suggesting improvement over the national estimates. This study glimpsed some of maternal socio-demographic, reproductive, pregnancy and health services related factors enhancing the risk of LBW in Bangladesh. Socio-economic factors like family income have an influence on birth weight [27,28]. Our result shows that a household income-expenditure profile is equally more likely to low birth weight babies compared to that household income-expenditure is surplus. The World Health Organization (WHO) has currently recommended birth spacing at least 24 months between the last live birth and the next pregnancy [29]. Both too short birth intervals or too long birth intervals lead to adverse maternal, neonatal and child health outcomes [30]. Our study depicts that the birth interval of the mothers less than 25 months markedly increases the risk of LBW infants that is consistent with previous studies [31]. In northern Tanzania, a shorter inter pregnancy interval (<24 months) was 1.61 times more likely to increase the risk of giving birth to an LBW baby compared with an inter pregnancy interval of 24–36 months [32]. In developing countries are higher proportions of underweight women for lower socioeconomic or ethnic or genetic predisposition. Also, in developing countries, underweight mothers were at enhanced risk of LBW babies [33]. Maternal dietary habits can directly influence the growing fetus [34]. Nutritional deficiencies women during pregnancy have the risk of giving low birth weight infants [35]. Body mass index has a more significant influence on LBW than the amount of weight gained during pregnancy [36]. Our finding reported that underweight mothers had 2.14 times higher risk of having LBW neonates (p=0.030). In 2019, a meta-analysis of China supports our results [37]. Nutritional status management of pregnant mothers has a strong role to lessen the LBW [38]. Analogous to hypervolemia, women generate an average of 30 to 40 ml of plasma per kilogram during the middle of the second trimester of pregnancy. Maternal anemia may develop and hemodilution arises when the number of hematological cells does not grow in similarity with this process [39]. Maternal anemia inclines the fetus to intrauterine increase limitation and may consequently manipulate the LBW [40]. Our results proved that women who had anemia problems during pregnancy associated a risk factor of low birth weight. Many studies have shown that maternal anemia is a risk contributor for LBW [41,42]. Study found that Bangladesh is one of the foremost countries for small gestational age at newborns [43]. We examined low birth weight was 2.50 times higher for preterm delivery (<37 weeks) than full term delivery ( ≥ 37 weeks).The finding is substantiated by a Bangladeshi study which depicted that LBW 8.92 times higher for Gestational age at preterm birth than term birth [16]. Preterm birth is the related factor with LBW [44]. Similarly, gestational age is considered as a significant contributor to birth weight in the United States [45]. Approximately half of all LBW infants are preterm birth in the most low and middle income countries [46]. Women who delivered preterm and were physically active (≥ 4 times per week) had decreased odds of having LBW infants [47]. Our research was not free from limitations. First, in the present study, we considered only mothers who had live births were interviewed and their babies assessed for low birth weight in Rajshahi district, Bangladesh. This study is an analysis of primary data, and as it is bound by the limitation of those data. Secondly, the study did not scrutinize some of the risk factors (e.g. mother’s smoking habits, mother’s pre-gestational BMI etc.). Thirdly, some comprehensive pregnancy history risk factors (such as maternal malaria, mother’s alcohol consumption, gestational diabetes, weight gain, infections as well as biological and genetic markers) were not included in the study. Obviously, more study will be required to give a more perfect answer for LBW children in Bangladesh.
We found Household income-expenditure profile; BMI of the mothers; Birth interval; anemia problems of the mothers during pregnancy period; and gestational age at delivery were identified as the most important associated with low birth weight of the neonates in Rajshahi district, Bangladesh. LBW risk could be reduced by the close and frequent follow-up of the field worker of health and family planning department, identify the risk mother, ensure ANC visit and medication supply, to adopt delivery planning and to maintain good nutritional status. Based on the study findings recommended the government of Bangladesh needs to strengthen its maternal health programs to address the focus on the modifiable factors associated with LBW. Decreasing the prevalence of LBW should endure to be a health priority of GOs and NGOs. Pregnant women and their household members have a role to avoid the LBW consequence by maintaining more antenatal care and unnecessary cesarean delivery. Hereafter, it is the need of the hour to reinforce the current maternal services at the community level to reduce LBW in Bangladesh. After all, immediate public health action is required for lessening LBW in Bangladesh.
Authors’ contributions
MAH created the concept; MAH, MSI, MRK and MJR created the design of the study. MAH, ASMAM, and MSI drafted the manuscript; MAH and MSI performed the statistical analysis; MGH and MAH made critical revisions of the manuscript. All authors read and approved the final version of the manuscript.
Acknowledgement
The authors gratefully acknowledge the authority of community clinic, Rajshahi, Bangladesh for giving permission to acquire the data. Finally, we would like to acknowledge the study participants, reviewers, and the academic editors of this manuscript.
Funding source
This study was conducted without any financial support from the funding body.
Conflict of interest
None to declare
Ethical approval
Ethical approval for this study was obtained from the Ethical Review Committee of Institute of Biological Sciences, University of Rajshahi, Bangladesh (No. 69/320/IAMEBBC/IBSC).
[Crossref][GoogleScholar][Pubmed]
[Crossref] [Google Scholar] [Pubmed]